CHHSM Advocacy Center
Vol. 8: Health Care Access

Marita’s Story

(Image description: Marita standing outside in front of a lake and trees on a sunny day. She is wearing a hat, red shirt, and jeans and is holding her son Reid, who is wearing a blue outfit.)
“Nilda’s classes were my sanctuary. Nilda has given me confidence in being a new mom. She has been a pillar of support. All I want to do now is to give back full circle–to support Nilda the same way she has supported us,” says Marita, who received care from, and is now giving back to, the Avondale Faith and Health Collaborative. The Collaborative is a partnership of faith-based organizations and communities that have come together to improve the health and well-being of Avondale residents and to share the strength already present in their Chicago neighborhood. CHHSM member organization Advocate Aurora Health, one of the 10 largest not-for-profit, integrated health systems in the United States, is a key partner in this collaborative. Marita attended classes to nurture and support new parents facilitated by Nilda Garcia, a Faith Community Nurse with Advocate. “I wasn’t prepared for that ‘fourth trimester,’ the first three months of becoming a new mother,” Marita said. “Nilda’s classes allowed me to connect with other mothers and helped me feel like I wasn’t alone.” She also worked with Ivette Menendez, Community Connector with Advocate, and received diapers and rent and utility assistance through the program. These additional supports are very intentional and speak to Advocate Aurora’s strong commitment to health equity by addressing social determinants of health. Whether someone has access to food, shelter, and clothing, for example, can have a direct impact on their health and their family’s health.
According to research conducted by the New York University School of Medicine, Chicago has the largest life expectancy gap in the country—where residents living in the Streeterville community are expected live to be 90, but just nine miles away in Englewood, the average life expectancy is only 60. “That is unacceptable,” says Bonnie Condon, Vice President of Community Health, Community Relations and Faith Outreach for Advocate Aurora Health. “Every man, woman and child deserves the chance to live a long and healthy life, regardless of where they live. Advocate Aurora Health is committed to narrowing that life-expectancy gap. We have put that commitment into action through our community strategy that addresses social determinants of health, such as food security, affordable housing, workforce development, healthcare access and community safety.”
An innovative and exciting example of this is Advocate Aurora’s implementation of NowPow, a mobile-enabled messaging and referral platform that gives the health system the ability to “prescribe” non-medical resources for their patients. Care managers and other providers have already been screening patients for needs around food, housing, transportation, and the like. The platform uses that screening in conjunction with a database of over 11,000 community services to connect patients with services specific for them in their neighborhood. Thus, it helps to close the loop between clinical and community service providers. The hospital can then truly be a center for healing—for the range of pains and ills one can experience in life—and does so not just for the community in which it is located, but with them. Condon affirms that this effort involves everyone from health care providers to faith communities, community organizations, and government partners to create and sustain the work that equity requires.
Definitions
Particularly coming from a social justice perspective, discussing health care access requires important distinctions in the language often used, and understanding the range of issues involved. To provide a foundation for this conversation, below are some helpful definitions from a variety of sources committed to this work.
- Health Care Access: the timely use of personal health services to achieve the best health outcomes. Access requires at least three main components: gaining entry into the health care system (usually through insurance coverage); accessing a location where needed services are provided in a timely manner (geographic availability); and finding a health care provider the patient trusts and can communicate with (personal relationship/cultural competency). When considering access, it is important to note that particular services can vary widely in terms of accessibility as defined here (e.g: a person could have health insurance but the needed abortion care is not covered by their plan and the nearest provider is located hours away).
- Universal Health Coverage: ensuring all people have access to the health services they need, when and where they need them, without financial hardship. It includes the full range of essential health services, from health promotion to prevention, treatment, rehabilitation, and palliative care. According to the World Health Organization, universal health coverage should be based on strong, people-centered primary health care. Good health systems are rooted in the communities they serve. They focus not only on preventing and treating disease and illness, but also on helping to improve well-being and quality of life.
- Social Determinants of Health: the conditions in which people are born, grow, live, work and age that impact one’s health. These circumstances are shaped by the distribution of money, power, and resources at global, national, and local levels. Social determinants of health are mostly responsible for health inequities—the unfair and avoidable differences in health status seen within and between populations due to past and current unjust policies.
Medical care is estimated to account for only 10-20 percent of the changeable contributors to healthy outcomes. The other 80 to 90 percent are social determinants of health, including but not limited to: social norms and attitudes (e.g: racism, homophobia, discrimination), exposure to violence, poverty, quality of education, safe and affordable housing, access to transportation, food insecurity, language literacy, employment opportunities, access to nature and environmental health, citizenship status, among many others.
Moreover, feedback loops exist among the social determinants of health. For example, poor health or lack of education can impact employment opportunities, which in turn constrain income. Low income reduces access to housing, food, and money for medications and treatments, decreasing well-being and increasing hardship. Hardship causes stress, which can increase risk to a variety of illnesses. Yet, while poverty is clearly a main contributing factor, it does not account for every disparity. For instance, Black Americans across the income spectrum are dying from preventable pregnancy-related complications at three to four times the rate of white Americans. Data has shown that other social determinants of health, like education level and socio-economic status, are not protective factors for Black Americans as they are for white Americans when it comes to maternal and infant mortality. The underlying variable is racism, which can manifest in the form of denial of care when enduring pain, to the long-term psychological toll of being Black in a racist society.
- Health Equity: the absence of avoidable, unfair, or remediable differences among groups of people, whether those groups are defined socially, economically, demographically or geographically, or by other means of stratification. Health equity implies that everyone should have a fair opportunity to attain their full health potential and that no one should be disadvantaged from achieving this potential. Further, health equity and health equality are not the same, though the words are often used interchangeably. Equality means giving everyone the same thing, whereas equity means giving people what they need to reach their best health.
- Health in All Policies: a collaborative approach to improving the health of all people by incorporating health considerations into decision-making across sectors and policy areas. The goal is to ensure that decision-makers are informed about the health, equity, and sustainability consequences of various policy options during the policy development process. A Health in All Policies approach identifies the ways in which decisions in multiple sectors affect health, and how better health can support the goals of these multiple sectors.
- Healing Justice: “a framework for how to holistically respond to and intervene on intergenerational trauma and violence, and to bring collective practices that can impact and transform the consequences of oppression on our collective bodies, hearts and minds,” according to Cara Page. Responding to the roots of trauma and injustice are understood as necessary for individual and collective healing. Healing Justice also aims to make healing accessible and culturally relevant for all people, and addresses who has access, or barriers, to these spaces and practices.
Coined by Cara Page and the Kindred Healing Justice Collective, this framework centers Indigenous, People of Color, queer, trans/gender non-conforming and disabled voices, and affirms that this work is rooted in the lineage of those communities. As such, a Healing Justice framework views healing as connected to social justice: “We understand that healing is a lifelong process and that often we never fully heal, especially when our loved ones are killed unjustly. We also understand that if we do not participate in a process of healing, the pain caused by state violence can overwhelm us as well as our communities. Holding these two truths we honor the need to be in healing processes, including the process of demanding justice for our loved ones… We support the healing of our communities not only because we deserve well-being, but also because the power required to win our people’s wellbeing is the power required to win all other visionary demands for justice.”
- Medicare: a federal program that provides health coverage for those 65 and older and for those who are under 65 and have a disability, no matter their income.
- Medicaid: a state and federal program that provides health coverage for those with limited incomes and assets. Each state uses financial eligibility guidelines to determine Medicaid eligibility, but the amount varies from state to state and program to program. For example, Medicaid-funded programs can be separated into various groups including older adults, people with disabilities, children, pregnant people, and caretakers of children. Some states also have programs for individual adults who do not fit any of these categories. A person can also be eligible for both Medicare and Medicaid and can enroll in both. Medicaid would then cover services that Medicare does not, like long-term care, and pick-up Medicare’s out-of-pocket costs (deductibles, coinsurances, copayments).
Background Information
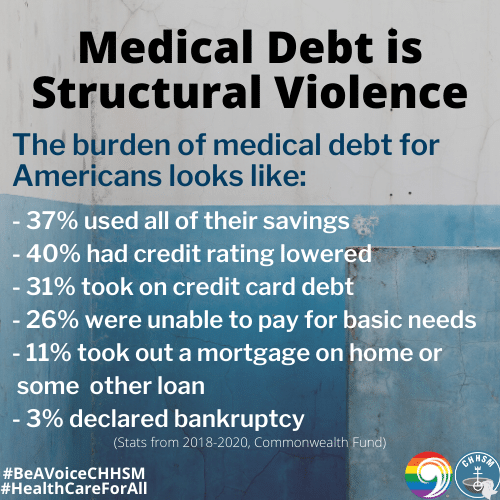
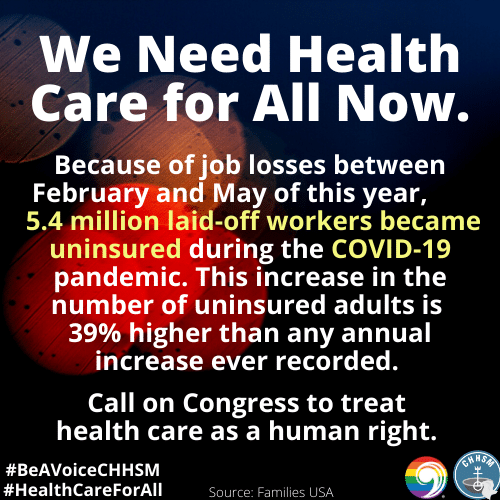
Advocacy for universal government-funded health care has been ongoing for nearly a century in the US, and this history is helpful to understand how we got to where we are today—where over 5 million American workers have lost health insurance due to the pandemic-driven recession and one-third of GoFundMe campaigns continue to be used to pay for medical bills.
In the late 19th and early 20th centuries, medical treatments were simpler, cheaper, and less effective than what we have today. Medical care was also unregulated. Physicians were more likely to treat patients in their homes, with the patients paying modest out-of-pocket fees; and hospitals, which functioned primarily to provide therapeutic-type care, were often run by religious and charitable organizations. Thus, the cost of the health care itself was not the main concern of the patients; it was the lost wages from not being able to work due to illness or injury. According to physician and author Elizabeth Rosenthal, “The earliest health insurance policies were designed primarily to compensate for income lost while workers were ill. Long absences were a big problem for companies that depended on manual labor, so they often hired doctors to tend to workers.”
As effective medical treatments and hospital standards grew in the 1920s, so did the cost of care and the concept of insurance. The model for many of today’s insurance plans can be traced to this period. In 1929 a group of Dallas schoolteachers contracted with Baylor University Hospital to receive up to 21 days of in-patient care a year for regular monthly payments of 50 cents. Similar prepaid service plans were popping up during the Depression era as well. Because the goal of these plans was not to make money, but rather to support patient savings and to keep hospitals functioning, state legislation allowed them to be categorized as nonprofit corporations with tax-exempt status. Within a decade, the model spread across the country and became known as Blue Cross Plans.
More robust insurance plans became needed, however, due to the rapid advancements in medical technology increasing the cost of care. During the same time, companies facing labor shortages found that offering health insurance attracted needed workers. And because the National War Labor Board froze salaries during and after World War II, the federal government supported these employer-based insurance plans and allowed for the money spent on employee health benefits to go untaxed—hoping for a win-win situation.
According to Rosenthal, an untended consequence of this led to the model of employer-based coverage and the boom of for-profit insurance companies, which were focused more on cash than on care. These for-profit plans accepted only younger, healthier patients, and charged varying rates, similar to the model of life insurance. This left many people unable to cover medical bills or to afford or even qualify for insurance if they were unemployed.
Yet, the idea of government-funded insurance was still part of the national conversation. Under multiple administrations from both political parties, several attempts to grant universal coverage were proposed and failed, such as Roosevelt’s Economic Bill of Rights, Truman’s Wagner-Murray-Dingell Bill, Nixon’s Comprehensive Health Insurance Plan, Rep. Dingell’s National Health Insurance Act, and Clinton’s Health Security Act to name a few. Rather than commit to a total health care reform, in 1965 Congress created Medicare and Medicaid programs to provide health care coverage to older adults, those who were poor, and eventually those with disabilities.
The next watershed health care legislation was the Affordable Care Act (ACA) signed into law by President Obama in 2010. By 2016, 20 million formerly uninsured Americans had acquired health care coverage through the new exchanges, the expansion of Medicaid eligibility in participating states, and federal subsidies to help lower- and middle-income Americans buy private coverage. The ACA mostly maintained the structure of coverage through Medicare, Medicaid, and employer-based insurance plans, but it made it so every insurer had to accept all applicants without charging based on pre-existing conditions or demographic status (except age).
Compared to before the ACA, fewer people are uninsured, but more people are underinsured, where they are left to shoulder the burden of high-deductibles and costs related to treatments and prescriptions not covered by their insurance. Research has shown that the greatest loss in the quality and comprehensiveness of coverage has occurred among people with employer-based plans. Of the 194 million U.S. adults ages 19 to 64 in 2018, 45 percent were inadequately insured. While the ACA’s employer mandate imposed a minimum coverage requirement on large companies, the requirement amounts to just 60 percent of a typical patient’s overall costs. Moreover, a gap remains for those who do not have insurance through employment and who are also ineligible for assistance, such as poor adults in states that did not expand Medicaid and undocumented immigrants, who are ineligible for Medicaid and the ACA.
Whether someone is uninsured or underinsured, barriers to health care access significantly impact one's overall health and quality of life. Lack of access leads to unmet health needs, delays in receiving appropriate care, diagnosis and treatment, the inability to get preventive services, financial burdens, preventable hospitalizations, and increased risk for premature death. Data from the Healthy People Midcourse Review demonstrate that there are significant disparities in access to care by sex, age, race, ethnicity, education, family income, and geography. For instance, US rural communities—from the Deep South, Appalachia, Alaska and Hawaii—face disproportionate health problems due to a lack of health professionals and quality medical services, issues related to transportation and remote locations, higher rates of poverty, and language or literacy barriers affecting medical decision-making and communication, to name a few.
As noted in the definitions above, health care access is also about the quality of care one receives after entering the health system, both through coverage and physically into a building. As such, it is essential to note the role racism—through racist policies and beliefs—continues to play in access disparities for People of Color. In the US, Communities of Color, particularly Black Americans, are considerably less likely to receive medical care when needed and when they do, they are more likely to receive a substandard quality of care. According to research, these disparities are evident in every sector of health care. For example, White patients with diseases such as cancer, HIV and diabetes were more likely to receive comprehensive and effective health care than patients of color with the same conditions. This has been shown to be true in maternal and infant mortality prevention, pain treatment and management, end-of-life care, and now COVID-19 treatment and prevention. However, research has also shown that Black babies are more likely to survive under the care of Black doctors and Black patients of all ages are more likely to get better medical care from Black doctors and nurses.
Racism is a long-standing public health crisis, and it is unsurprising that health care has historically been a racialized issue. Although consistent and strong opposition by the American Medical Association and fear-based associations with communism have been key reasons why universal health care has been blocked, more recent research speaks to how racist ideas factor into racist health policies. In his book Dying of Whiteness, physician and researcher Jonathan M. Metzel explains how the frameworks of White racial resentment have shaped attitudes towards public policy—particularly toward health care access—which not only lead to an increase in mortality rates for People of Color, but for the White voters who support the very policies that are killing them too.
As Metzel exemplifies through a patient narrative: “Ain’t no way I would ever support Obamacare or sign up for it,” he told me. “I would rather die.” When I asked him why he felt this way even as he faced severe illness, he explained: “We don’t need any more government in our lives. And in any case, no way I want my tax dollars paying for Mexicans or welfare queens.” Suffice it to say, now more than ever is the time to bring a racial and health equity lens to health care policy and practice.
Current Context
The Affordable Care Act has been credited with reducing the racial and ethnic disparities that exist in access to insurance and health care. With the expansion of access to insurance as well as Medicaid eligibility, progress was made in narrowing the gap between Black and Brown insurance rates and white insurance rates. It is stunning then, to see the current administration working hard toward a wholesale dissolution of the Affordable Care Act and how it has been doggedly pursuing this goal in the courts. It has also used the regulatory process to reduce access to insurance and Medicaid. For instance, the administration has now implemented work requirements that are particularly onerous for many folks who need access to Medicaid—which in turn widens the racial disparities in health care access. In Mississippi, 71 percent of adults who would be effected by work requirements for Medicaid are Black. This is unsurprising, though, given that work requirements are inherently racist, as their implementation and implication stem from a white supremacist justification for slavery.
At every turn the administration has used every tool at their disposal to reduce access to insurance and medical care and has continued to deepen the existing disparities that exist in care for Black and Brown people. If the ACA were to be repealed, nearly 30 million people would lose their insurance and health care access immediately. And the protections that currently exist for pre-existing conditions and very costly medical care would cease to exist, with no legislative plan for replacement. There are a number of legislative proposals that aim to increase health access, but we need to consider how those plans either build off of inequitable systems, or how they work to reshape them.
Health care access is multifaceted and should encompass a wide range of factors when evaluating it. It means adequate access to food and shelter; it means mental health, vision, and dental care. As discussed in the background section, health care access is more holistic than many policy makers consider it to be. This is why as we look at our candidates, we need to think about leadership that will consider the whole person and society as a whole, rather than relying on how things have always been done.
A Faith-Based Response
Heal the sick, raise the dead, cleanse those with skin diseases, drive out demons. You have received free of charge; give free of charge (Mt: 10:8-9). For nearly four decades, the United Church of Christ has advocated for health care as a human right and priority for all people. In recent years, this vision has been articulated through General Synod resolutions like An Urgent Call for Advocacy in Support of Health Care for All (2009), the Ten Priorities for a Faithful Health System (2017) co-authored by UCC Justice and Witness Ministries and the Washington Interreligious Staff Community, advocating directly in the halls of the Capitol, and endorsement of the Medicare for All Act of 2019. It is also found in how the UCC invests its money. Through United Church Funds, investments are made with the ethical life of a company in mind, with access to health care and responsible pharmaceutical pricing used as a screening strategy.
CHHSM member organizations and UCC congregations are working locally to improve health care access for their communities in innovative and significant ways. A powerful example of this comes from St. Louis, MO, where Deaconess Foundation, Deaconess Nurse Ministry, and Epiphany UCC are all connected through this issue. Epiphany UCC is home to one of the Salam Clinics, a free health clinic with nursing support from Deaconess Nurse Ministry. It also provides office space for staff members of Missouri Health Care for All—an organization dedicated to grassroots mobilization on health care issues—which receives funding and support from Deaconess Foundation, as one of their Just for Kids Anchor Institutions. Their work saw a major victory in August when the voters of Missouri approved Medicaid expansion, giving coverage to 230,000 more people in the state after years of strong opposition.
That is not the only major celebration connected to the collaborative work of Deaconess Foundation. This year they were recognized as the Health Advocacy Organization of the Year by the St. Louis American, in part due to their campaign to cancel medical debt for low-income households in St. Louis. Rev. Traci Blackmon, senior pastor at Christ the King United Church of Christ and Associate General Minister of Justice and Local Church Ministries, came to the foundation with the idea of participating in RIP Medical Debt, and Deaconess gave its full support. Donations from across the UCC amounted to $60,000 and Deaconess Foundation gave an additional $40,000. With that $100,000 donation, they purchased $12.9 million in medical debt of families living at or below the poverty line. Rev. Blackmon also engaged the CHHSM Board and staff around this issue, and for the UCC’s Giving Tuesday, CHHSM donated $15,000 to the nation-wide campaign.
Also in St. Louis is CHHSM member iFM Community Medicine, which takes health care services directly to the points of need in the community and overcomes access barriers related to cost, transportation, language, and trust. iFM has 20 on-site clinics throughout the city in schools, shelters, and other social service organizations. As such, its work is inherently collaborative and responsive to the needs that emerge within these relationships. This has certainly been the case with other CHHSM member organizations in St. Louis. For example, in 2017 iFM and Deaconess Nurse Ministry partnered with St. Andrew’s, a low-income older adult housing facility, and Every Child’s Hope, a ministry for children who have experienced trauma, to provide vital medical services to these communities. “So often, agencies work independently, trying to do all things,” says Donna Smith-Pupillo, executive director of Deaconess Nurse Ministry. “However, the community and people are served more holistically when the work is done in a collective, collaborative way.” And in the midst of COVID-19, iFM is being looked to by schools for their expertise as re-opening plans take shape and is partnering with youth shelters to develop on-campus and drive-through testing to make admissions safer and easier.
Questions for Candidates
- Are you aware of the ways in which work requirements for Medicaid widen the racial inequity gap in health care access?
- What plans do you have for protecting health care access?
- What plans do you have to improve access in an equitable way?
- What does equitable health access mean to you?
Social Media Samples
You can find the below graphics and more by following CHHSM and JWM on social media.
Follow the UCC’s Council for Health and Human Service Ministries (CHHSM) at:
Follow the UCC’s Justice and Witness Ministries (JWM) at:
More Information
For more on health care access and health equity, check out these resources:
- Health and Human Service Sunday Liturgical Elements and Prayers by CHHSM
- Healing Justice Toolkit by Dignity and Power Now
- Medical Apartheid Book Discussion Guide by Academic Life in Emergency Medicine
- Health in Prisons: A World Health Organization Guide to the Essentials of Prison Health
- Health Justice Activist Starter Kit by Physicians for a National Health Program
- The Physician Advocate: Advancing Policies that Support Health Equity by The EveryONE Project
- An Introduction to Health in All Policies by the American Public Health Association
- Health Literacy Universal Precautions Toolkit by the Agency for Healthcare Research and Quality
- Medicaid Eligibility and Enrollment Toolkit by the Centers for Medicare & Medicaid Services
COVID-19 and Health Care Access
The spread of the COVID-19 virus has caused changes in access to health care and services. Below are some relevant resources that are specific to COVID-19.
- COVID-19 Health Equity by the US Department of Health and Human Services
- COVID-19 and the Criminal Justice System by the Prison Policy Initiative
- COVID-19 Partner Toolkit by the Centers for Medicare & Medicaid Services
- COVID-19 One Stop Shop Toolkits by the Centers for Disease Control
CHHSM Organizations involved in Health Care
CHHSM has 3 member organizations whose primary focus is to provide primary and acute care health services including:
Where to Find Us
Please visit our websites to learn more about CHHSM and JWM.